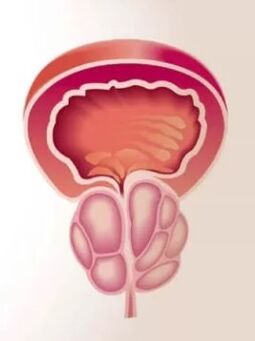
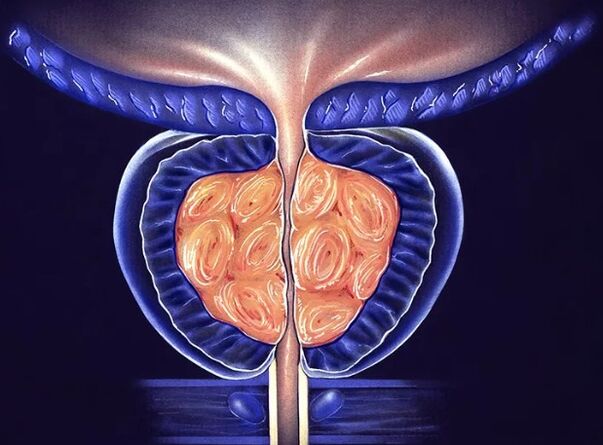
Prostatitis is the most common urological pathology in men of reproductive age. According to polls, every third of them has experienced symptoms at least once in their lives that can be interpreted as prostate inflammation. Despite such a high onset of pathology, prostatitis remains a poorly studied disease.To this day, there is no consensus that it is becoming an initial factor for inflammation, as it is possible to distinguish pathogens of PPI from the genital tract of patients only in 10% of cases. The lack of clear diagnostic criteria and characteristic signs of the disease complicate patient reporting. The symptoms of prostatitis are so nonspecific that each doctor interprets them with a large share of subjectivity and can attribute it to a completely different pathology. Accordingly, the approach to treatment also varies and often patients wander from one hospital office to another without positive dynamics for years. Prostatitis deprives a person of confidence in his sexual power, attaches his thoughts for a problem and brings him not as physical as psycho -emotional suffering. The prostate gland (prostate) is a small glandular organ of a person located around the urethra under the bladder. It tightly waves the urethra, forming one of its sphincters - a muscle jack designed to hold the urine. In its shape and size, the prostate looks like a brown nut that is often compared to anatomists. The part of the urethra that passes inside the gland is called prostatic. Its posterior convex part of the prostate is in contact with the rectum, so it can easily be felt with a rectal examination of the finger. The anterior surface of the gland is close to the pubic joint and is connected to it with moving connections of the connective tissue, and the venous split is located between them. The prostate gland consists of lobules, each of which is made of alveoli - small bags lined with a secret epithelium. The alveoli are connected to each other by the outlet channels in the form of pipes that merge with each other, expand and eventually fall into the part of the Simpletle urethra. Inside secretory bags, prostate juice is synthesized and accumulated, which includes nutrients for sperm. It allows male sex cells to maintain their activity in the female body for up to 5 days, which greatly increases the chances of fertilizing. Enlightenment of the gland occurs during ejaculation. Prostate juice is mixed with the secret of the testes and represents 10 to 30% of the final volume of semen. Thus,The prostate gland performs 2 main functions in a person's body: Prostatitis is an inflammatory changes in the prostate gland and it should be understood that they occur not only under the influence of bacterial microflora.The causes of inflammation can be any factors leading to damage to the tissue of the gland and the destruction of its cells. As in all other tissues, the inflammatory process in the prostate takes place at certain stages: For the reason, prostatitis is divided into: The easiest to diagnose acute prostatitis,Which continues with signs of intoxication and pronounced inflammation. In humans, the temperature rises sharply to 38-39 degrees C, with a pronounced pain in the perineum, in the rectum area. They can give in the groin, in the penis testis and be so unbearable that a person's daily activity is abruptly disturbed. In some cases, the body temperature measured in the axillary cavity does not exceed normal indicators, but the rectal will in any case be 1-2 degrees normal. The signs of prostatitis also turn into a violation of urination: severe desires for urination, after which it is impossible to limit or sharp slowing of urine due to severe edema of the gland. Sometimes bowel movements become painful, as the prostate, enlarged in size, sticks out in the lumen of the rectum. Chronic prostatitisIn its manifestations, it is so diverse that it can easily be confused with another pathology. In the most typical cases, the symptoms of prostatitis are presented: As a rule, with chronic prostatitis, the general well -being of a person is not disturbed, the body temperature is preserved normal throughout the disease. The diagnosis is established by the medical urologist or andrologistAfter examination of the patient, collecting anamnesis and studying symptoms. The doctor should detect the patient's contraception method, the presence of PPI in a sexual partner, the possibility of anal contacts without a condom. These data facilitate the diagnosis and direct the doctor's thoughts in the right direction. The prescription of the symptoms of the disease or discomfort in the perineum allows us to evaluate the course of prostatitis and its severity. The urologist necessarily examines the patient's genital organs and conducts rectal examination of the prostate gland. To do this, he inserts a finger into the back passage of the patient and Marie the standing out prostate on the anterior wall of the rectum. The soreness and its size indicate the intensity of the inflammatory process. The doctor also conducts a number of instrumental, microscopic, bacteriological and immunological studies to clarify the cause of the disease. The most common diagnostic method is a 4 or 3 glass urine sample. The first method is more time -a large and difficult to practice in practice, as it requires the patient several times to deliberately interrupt urination. The second modification is more: the patient constantly urinates in three different containers in equal parts. The first part speaks to the condition of the urethra, the second about the pathology of the bladder and the kidneys, the third obtains information about the state of the prostate gland. All materials collected are studied under a microscope. With prostatitis in the third part of the urine, leukocytes and sometimes bacteria are detected. Access to prostate and massage examination when collecting secrets The secret of the prostate gland is also taken for microscopy.To do this, the doctor performs prostate massage through the wall of the rectum for a while so that it is emptied into the urethra. The smokes are made from the collected material in the laboratory, painted and studied with a large increase. The sign of inflammation is leukocytes, bacterial etiology of the disease - bacteria when spreading. In order to determine the type of pathogen, prostatic secret is sown in nutritional environments. If it contains pathogenic microorganisms, then after 3-5 days they form microbial colonies, which can then be studied by the bacteriological method, allows you to receive data on the sensitivity of the microflora to antibiotics. Of instrumental diagnostic methods, : Starting the treatment of chronic prostatitis, you should adjust to a long fight as it is not always possible to cure it in a few weeks or even months. It is recommended to combine various methods and tools for therapy, it is useful to improve household drug therapy. Stagnant prostatitis requires regular sex, interrupted sexual acts are unacceptable. The psycho -emotional origin of the patient is important: depression, depression, personal problems and sexual sphere are able to cancel all the efforts of doctors. Prevention of prostatitis includes: Despite the fact that prostatitis is not related to the risk of developing adenoma or prostate cancer today, the disease carries a lot of suffering to its owner. A man exhausted by chronic pain, feeling his sexual weakness, tired of prolonged treatment, changes a noticeable external and experienced doctors determine such patients at first glance. In order to avoid such fate, you must be careful about your health carefully protected with each new partner and treat sexually transmitted diseases on time. Prostatitis is not completely treated in all cases, but an experienced urologist is able to significantly improve the patient's condition and quality of life.